Advanced Care At Home (ACAH) is coming to the GSAA and that date is July 9th.
Here is a quick refresher on what ACAH is and how it affects us.
- What is ACAH? A program that takes care of patients who meet inpatient criteria but are stable enough to be managed at home. Think your failed CDA patients, cellulitis patients who failed oral therapy, CHF patients who need IV diuresis with stable oxygen requirements, neutropenic fever patients, etc. It is NOT the same as a discharged patient on home health. These patients are seen at least daily by nurses and virtual ACAH physicians. Labs (within 4 hours) and imaging are available. Patients are set up with technology to allow them to stay connected to the medical hub and communicate their needs.
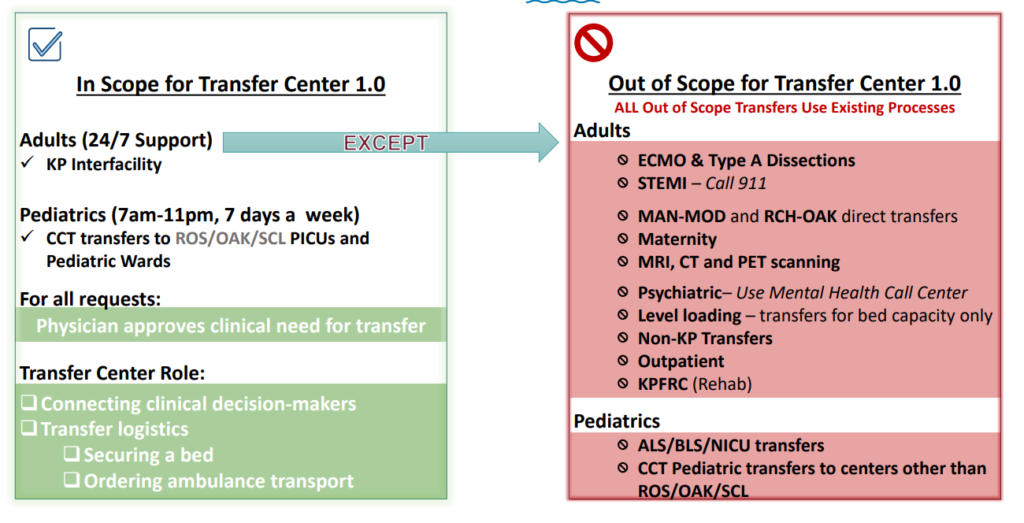
- How it affects us: Patients that normally need admission who are candidates for ACAH may be transferred directly from ER to ACAH (without HBS involvement). Patients on your panel may be discharged sooner to ACAH.
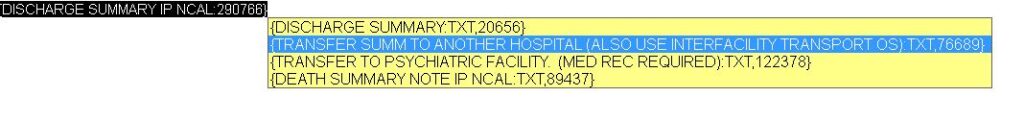
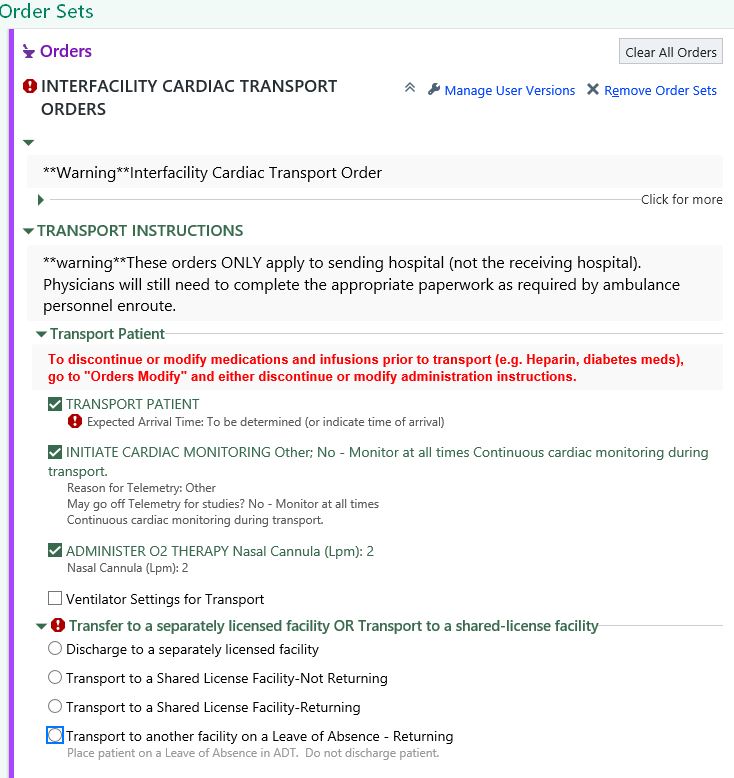
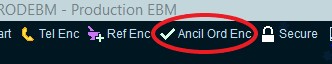
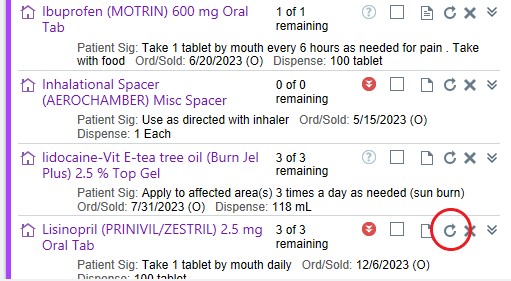
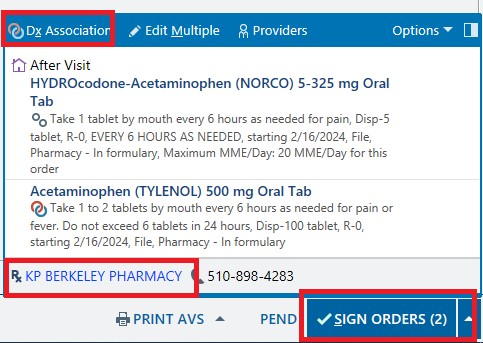
- HBS roles and responsibilities: Screen through your list daily to see if there are any candidates for this program. Inform your PCC and ACAH Hospitalist to review case for ACAH admission. If approved, complete POLST, discharge summary, and order for DC to ACAH (DCI and AVS not needed).
There will be a formal presentation during our next department meeting. For now feel free to review the following powerpoints.